With almost no exception, you see cases of Osteoarthritis (OA) – the most common type of, if not virtually synonymous with, Degenerative Joint Disease (DJD) — every week in your clinic. Depending on the source, OA is reported to affect between 6-25% of animals in the general population, with that number growing at alarming rates.
As a degenerative disease, i.e. one that gets irreversibly worse with time, it is critical to catch the condition early and act quickly. This article outlines the three fundamental steps to keep your patients on all-fours:
- Look: Your pet owners can help with awareness at home
- Find: Digital Radiography can help to see inside that inflamed joint
- Treat: Laser Therapy can help to Stop Inflammation, Reduce Pain, and Increase Mobility.
Obviously the battle against OA begins with early detection, and that happens well before the patient ever comes to the clinic. A recent study performed by Banfield, with their wealth of patient data across their thousands of hospitals, uncovered some very highly-correlated warning signs, most notably related to bodyweight and obesity.

Perhaps the most insightful concept is that obesity can be both the cause AND the effect of osteoarthritis. After all, an over-weight dog will certainly have more strain on its joints, leading to wear-and-tear on the cartilage that slowly erodes away, causing the joint disease. And on the other hand, if an animal is experiencing pain or limited range of motion in their joints, they will be less likely to exercise and thus more likely to pack on the pounds
According to the study results:
- 52% of dogs and 41% of cats with osteoarthritis are also overweight or obese
- Overweight or obese dogs are 2.3x more likely to be diagnosed with OA
- Dogs with OA are 70% more likely to be overweight or obese
Other indicators around the house, both for cats and dogs, include any reluctance to go up steps, jump onto the bed, or keep up while on a leash. Even things as subtle as posture while sitting or tenderness to be pet around a joint can be early signs of OA. Older animals and even specific breeds are more likely to develop joint disease.
To read more about Banfield’s study on OA as well as a list of at-home preventative measures, click here.
FIND IT, with Digital Radiography
Beyond physical examination and behavioral analysis, Digital Radiography (DR) is the first and most effective tool in your diagnostic arsenal to identify osteoarthritis in a patient.
The hallmark radiographic features of osteoarthritis are the presence of osteophytes, bony outgrowths from the margins of the joints. Other features in more advanced cases include erosions of subchondral bone and narrowing of joint spaces due to articular cartilage erosion.
A major advantage of digital radiography is the ability to visualize soft tissues and bony structures in the same image. Increased intra-articular soft tissues are easily assessed (joint effusion, synovitis), and may be the only radiographic sign early in the course of osteoarthritis or injury (cranial cruciate rupture, meniscal tear). Additionally, periarticular soft become thickened from fibrosis as the body attempts to stabilize the joint also well visualized with digital radiography.
Radiologist Tip
As always in radiographic assessments, orthogonal views (e.g., lateral and craniocaudal) are useful to fully assess osteoarthritis, as different portions of the joints are highlighted. For example, on a lateral view of the dog stifle, osteophytes are commonly seen on the apex of the patella and along the femoral trochlear ridges, the tibia may be positioned cranial to the femur (cranial tibial thrust), and an increase in soft tissue within the joint can be seen cranially (“loss of infrapatellar fat pad”) and bulging caudally. The craniocaudal view allows excellent assessment of the tibial plateau and the femoral epicondyles, where osteophytes of the medial and lateral margins are common.
TREAT IT, with Laser Therapy
Laser therapy is arguably the single most effective, non-pharmaceutical device for the treatment of inflammation. And osteoarthritis, by definition, is an inflammatory issue, regardless of its primary or even secondary causes.
To get a little technical, here is a paragraph from the latest (soon-to-be-printed) textbook on the subject:
Acute joint inflammation decreases with laser therapy (LT) due to the reduction in the pro-inflammatory mediators IL-1, COX-2, TNF, and IL-6. LT can also reduce the inflammatory infiltrate; in osteoarthritis models, for instance, it decreases polymorphonuclear cells in the synovial fluid and capsule. The resolution of the inflammation is further enhanced with the production of substances such as TGF-β, both in healthy and experimentally-induced diabetic models. Besides, LT can decrease the above-mentioned MMP levels to inhibit cartilage degradation – specifically MMP-2, MMP-3, MMP-9, and MMP-13.
To learn more about these biomarkers and inflammatory mediators, get citations for some of these results, or just learn about laser therapy in general, the book will be published this fall: Click here to pre order on Amazon, and in the meantime you can click here to contact the author.
From more of an implementation perspective, OA is one of the top five “bread and butter” conditions commonly treated with laser in a veterinary practice. It is even listed on the ACVS website on osteoarthritis in dogs as one of the rehab modalities.
For the more chronic presentations, the treatment plan includes more of a “front-loaded” regimen where you treat six times over three weeks: three times the first week, twice the second week, and once the last week. From there this usually turns into a maintenance package of once every 3-4 weeks as necessary and to stay in front of it.
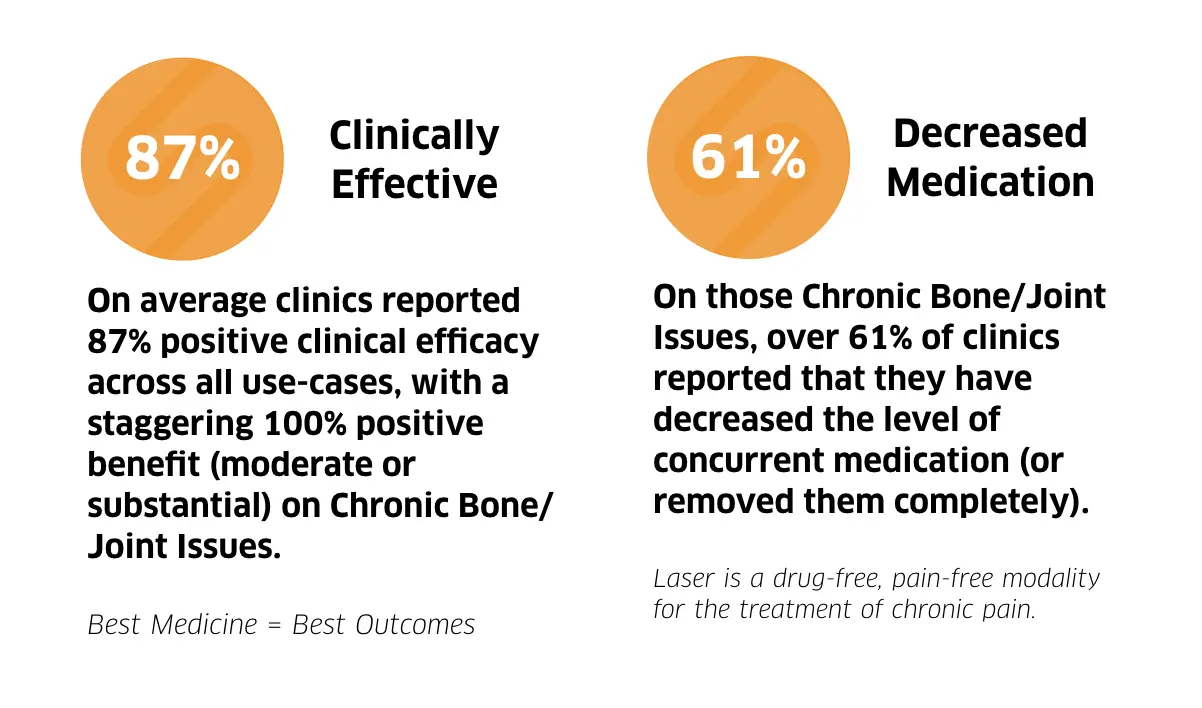
SOUND recently did a survey of its entire laser install base, and when asked about chronic bone/joint issues, a staggering 100% of respondents reported positive clinical benefit from laser therapy (64.71% moderate and 35.29% substantial), with zero reports of adverse (or even minimal) response. On top of that, 61% of respondents reported that as a result of incorporating laser therapy to the treatment, they were able to decrease the dosage of concurrent pain/inflammation medications used. This is of ENORMOUS benefit to the patient’s liver, kidneys, and overall quality of life.
To learn more about the results of this study, click here.
Take Home Message
Osteoarthritis is prevalent, has been growing, and has no signs of stopping. According to Banfield’s study, there has been a 66% increase in the diagnosis of OA in dogs, and 150% in cats, over the last 10 years. That said, having the right equipment to Find It and Treat It can go a long way in increasing quality of life and extended the lives of your pets.
To learn more about SOUND’s Digital Radiography solutions click here and Laser solutions click here, or call 800-268-5354.

